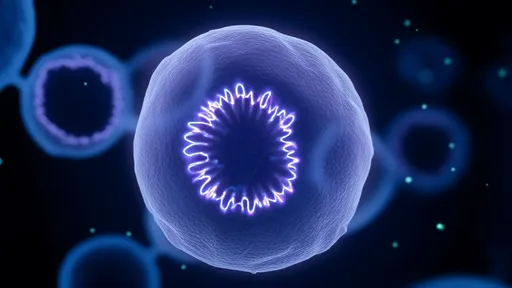
In a groundbreaking discovery that could reshape our understanding of chronic pain, scientists have identified a previously unknown mechanism within glial cells that acts as a hypersensitivity switch in the nervous system. This biological amplifier, hidden within the intricate network of non-neuronal support cells, appears to dramatically intensify pain signals under certain conditions. The findings, published across several high-profile journals, are sending ripples through the neuroscience community as researchers grapple with the implications for millions suffering from persistent pain conditions.
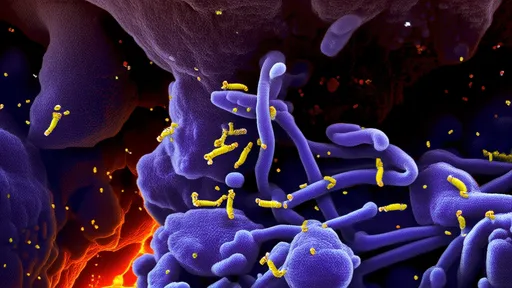
The glial cells, long considered mere "glue" holding neurons together, have emerged as active participants in pain modulation. These star-shaped astrocytes and microglia possess the startling ability to dial up neural sensitivity through complex chemical signaling. When triggered by injury or inflammation, they enter a hyperactive state that effectively lowers the threshold for pain perception. This creates a vicious cycle where even mild stimuli become excruciating, a hallmark of conditions like fibromyalgia and neuropathic pain.
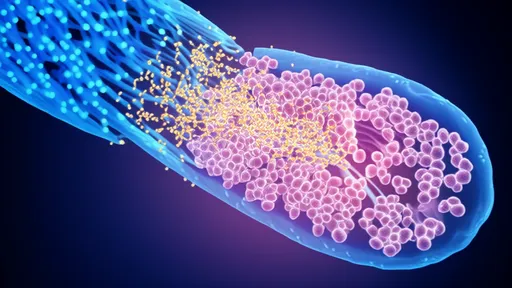
Researchers at multiple institutions have independently observed this phenomenon using advanced imaging techniques. What they've captured are glial cells undergoing dramatic morphological changes when exposed to inflammatory markers. The cells extend their processes toward synapses, releasing a cocktail of signaling molecules that potentiate neuronal firing. This glial-neuronal crosstalk appears fundamental to the development and maintenance of pathological pain states - a revelation that challenges decades of neuron-centric pain research.
The signaling cascade involves several unexpected players. ATP molecules, typically associated with cellular energy, serve as distress signals when released in the extracellular space. Glial cells detect these molecular cries for help through specialized purinergic receptors, triggering their transformation into pain-amplifying machines. Meanwhile, pro-inflammatory cytokines like IL-1β and TNF-α act as chemical messengers in this cellular conspiracy, creating an environment where pain signals gain unnatural strength as they travel toward the brain.
Perhaps most intriguing is the discovery that this hypersensitivity switch isn't binary - it operates more like a dimmer with multiple settings. The intensity of glial activation corresponds directly with the degree of pain amplification, suggesting a graduated response system that could explain why pain chronification occurs differently across individuals. This nuanced understanding opens doors for personalized pain management approaches tailored to a patient's specific glial reactivity profile.
Clinical implications are already beginning to emerge from laboratories. Several pharmaceutical companies have glial-modulating compounds in various stages of development, targeting specific points in this newly mapped signaling pathway. Early trials show promise in conditions previously considered treatment-resistant, offering hope where traditional analgesics have failed. The approach represents a paradigm shift from silencing neurons to calming the overzealous glial cells that drive their hyperactivity.
Neuroscientists caution that much remains unknown about the long-term consequences of manipulating glial function. These cells perform vital roles in neural maintenance and protection, raising questions about potential side effects of sustained intervention. Researchers emphasize the need for therapies that restore balanced glial activity rather than completely suppressing it, drawing parallels to immune modulation strategies that have revolutionized autoimmune disease treatment.
The discovery also sheds light on why certain existing medications provide unexpected pain relief. Drugs like minocycline and propentofylline, developed for entirely different purposes, exhibit glial-modulating properties that may explain their off-label efficacy. This retrospective understanding is accelerating the identification of promising drug candidates through computational analysis of known compounds' effects on glial pathways.
Beyond pharmaceuticals, the findings suggest novel non-invasive approaches could emerge. Early experiments with specific light wavelengths and electromagnetic fields show potential to gently modulate glial activity without chemical intervention. Such techniques, if perfected, could offer pain relief without the side effect profiles of systemic medications - particularly appealing for vulnerable populations like pregnant women or elderly patients.
The societal impact of this research cannot be overstated. Chronic pain affects approximately 20% of adults globally, with economic costs rivaling those of cancer and heart disease combined. By addressing the root cause of pain amplification rather than just symptoms, glial-targeted therapies could dramatically improve quality of life while reducing reliance on opioids and other problematic analgesics. Pain specialists anticipate a new era in management strategies that prevent sensitization rather than merely coping with its consequences.
As research progresses, attention is turning to why this amplification system evolved in the first place. Some theorists propose it served an important protective function in our evolutionary past, enforcing immobilization during healing. In modern contexts where prolonged rest isn't always practical or necessary, this once-advantageous mechanism becomes maladaptive. Understanding these evolutionary roots may inform more natural approaches to resetting the system.
The discovery also raises fascinating questions about individual differences in pain experience. Variations in glial reactivity could explain why some people develop chronic pain after minor injuries while others recover completely from significant trauma. Ongoing genetic studies are mapping polymorphisms in glial-related genes that might predict susceptibility, paving the way for preventive strategies in high-risk individuals.
While much focus remains on pharmacological solutions, integrative approaches are gaining scientific credibility. Practices like mindfulness meditation and controlled breathing exercises appear to subtly influence glial activity through the vagus nerve, providing a biological explanation for their pain-relieving effects. This convergence of ancient wisdom and modern neuroscience is fostering innovative hybrid therapies that combine technological and holistic elements.
The road from laboratory discoveries to clinical applications remains long, but the pace of progress is accelerating. With major funding initiatives supporting glial research and unprecedented collaboration between academic institutions and pharmaceutical developers, many believe we stand at the threshold of a revolution in pain management. For millions whose lives have been constrained by persistent pain, these developments offer more than hope - they illuminate a concrete path toward reclaiming comfort and functionality.
As research continues to unravel the complexities of glial signaling, one thing becomes increasingly clear: the nervous system's support cells are anything but passive. In their intricate dance with neurons lies the key to understanding - and ultimately controlling - one of medicine's most persistent challenges. The pain amplification switch, once flipped, may not need to remain permanently on. Science is now learning how to gently return it to its proper setting.

By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025