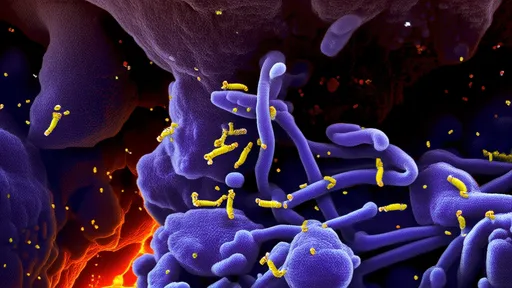
In the relentless battle against cancer, scientists are turning to an unlikely ally—engineered bacteria. These microscopic soldiers, reprogrammed to seek out and destroy tumor cells, represent a paradigm shift in oncology. Unlike traditional treatments that indiscriminately attack dividing cells, these living therapeutics exploit the unique biology of tumors to deliver lethal payloads with precision. Recent breakthroughs in synthetic biology and microbiome research have transformed this once-fanciful concept into a promising clinical reality.
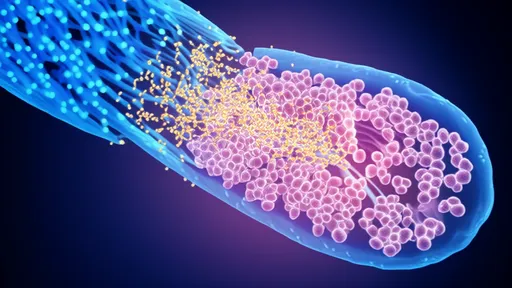
The human body hosts trillions of bacteria, many of which naturally colonize tumor microenvironments. Researchers have harnessed this tropism by genetically modifying non-pathogenic strains like Escherichia coli and Salmonella to serve as targeted drug delivery vehicles. These engineered microbes can penetrate deep into tumor cores, areas often inaccessible to conventional drugs due to poor vascularization. Once inside, they act as microscopic factories, producing anti-cancer toxins directly at the malignancy site while sparing healthy tissue.
Precision Warfare at the Cellular Level
What makes bacterial vectors particularly remarkable is their ability to sense and respond to tumor-specific conditions. Scientists have equipped these microbes with genetic circuits that activate toxin production only when encountering hypoxia (low oxygen), acidic pH, or other biochemical hallmarks of cancerous growth. Some strains even carry "suicide switches" that trigger bacterial self-destruction after toxin delivery, addressing safety concerns about persistent colonization.
The toxin arsenal deployed by these microbial allies includes traditional chemotherapeutic agents like doxorubicin, as well as novel protein toxins derived from nature's deadliest organisms. Pseudomonas exotoxin A, diphtheria toxin fragments, and even spider venom peptides have all been successfully produced by tumor-colonizing bacteria. Early-phase clinical trials demonstrate these living drugs can shrink tumors resistant to radiation and chemotherapy, with some patients achieving durable remission.
Overcoming the Tumor Fortress
Solid tumors erect formidable defenses against treatment—dense extracellular matrices, immunosuppressive microenvironments, and cellular heterogeneity that fosters drug resistance. Engineered bacteria circumvent these barriers through multiple ingenious mechanisms. Certain strains secrete enzymes that degrade the tumor's protective scaffolding, allowing better penetration of therapeutics. Others produce cytokines that recruit and activate the patient's own immune cells, creating a combined assault on the malignancy.
Perhaps most impressively, some bacterial therapies address the fundamental challenge of cancer metastasis. Researchers at leading institutions have created "sentinel strains" that circulate through the bloodstream, identifying and marking microscopic secondary tumors before they become detectable by conventional imaging. These microbial scouts could revolutionize early intervention strategies for aggressive cancers.
The Safety Paradox
While the idea of introducing bacteria into cancer patients may raise concerns, decades of research have established rigorous safety protocols. The strains selected for engineering are either attenuated pathogens or commensal bacteria with proven biosafety profiles. Advanced containment strategies, including auxotrophy (making bacteria dependent on supplied nutrients not found in healthy tissue) and antibiotic-sensitive kill switches, ensure precise control over microbial activity.
Clinical experience reveals an unexpected benefit—the bacterial component itself often stimulates potent anti-tumor immunity. The immune system, evolved to combat microbial invaders, mounts a vigorous response against both the engineered bacteria and the adjacent cancer cells. This bystander effect enhances the therapy's effectiveness and may provide long-term immunological protection against recurrence.
From Lab Bench to Bedside
The translation from animal models to human trials has progressed rapidly. Several biotech companies now have engineered bacterial therapies in Phase II trials for pancreatic, colorectal, and glioblastoma cancers—some of the most treatment-resistant malignancies. Early results show improved progression-free survival with manageable side effects, primarily low-grade fever and transient inflammation at tumor sites.
Regulatory agencies have established new pathways to evaluate these living drugs, recognizing their unique properties differ fundamentally from chemical pharmaceuticals. The FDA's recent approval of a bacterial-based therapy for bladder cancer marks a watershed moment, paving the way for more sophisticated microbial anti-cancer agents.
The Road Ahead
Future developments aim to create "smart" bacterial systems that adapt their therapeutic approach based on real-time tumor response. Teams are working on quorum-sensing networks that allow microbial populations to coordinate toxin production based on tumor burden. Other groups are engineering bacteria to deliver gene-editing tools capable of permanently disabling oncogenes within cancer cells.
As with any emerging technology, challenges remain. Optimizing dosing schedules, preventing neutralization by the immune system in repeat administrations, and ensuring consistent tumor colonization across diverse patients represent active areas of investigation. Nevertheless, the field has progressed from speculative research to clinical application at remarkable speed.
The convergence of microbiology, genetic engineering, and oncology has birthed a transformative approach to cancer treatment. These microbial armies, invisible to the naked eye but mighty in their therapeutic potential, exemplify medicine's growing ability to harness nature's complexity in the fight against humanity's most persistent foe. As research advances, engineered bacteria may soon become standard weapons in the oncologist's arsenal, offering hope where conventional therapies have failed.

By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025