The human genome is a vast and intricate landscape, harboring not only the genes that define our biology but also remnants of ancient viral infections that have shaped our evolution. Among these remnants, human endogenous retroviruses (HERVs) stand out as silent witnesses to a long-standing battle between viruses and their hosts. Once considered "junk DNA," these viral fossils are now emerging as key players in autoimmune diseases, raising provocative questions about their role in health and disease.
For decades, scientists dismissed HERVs as genetic debris—leftovers from infections that occurred millions of years ago. These retroviral sequences, accounting for nearly 8% of the human genome, were thought to be harmless relics of our evolutionary past. However, recent research has uncovered a startling truth: under certain conditions, these dormant viral elements can awaken, triggering immune responses that may contribute to autoimmune disorders such as multiple sclerosis, lupus, and rheumatoid arthritis.
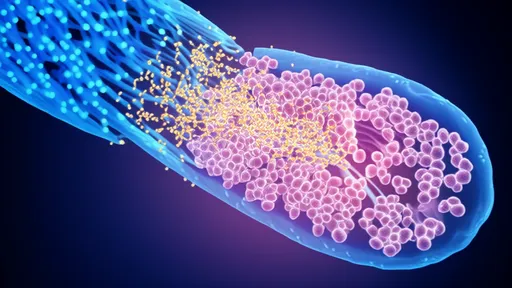
The reawakening of HERVs is not a random event. Environmental factors, including infections, stress, and epigenetic changes, can strip away the molecular locks that keep these viral sequences silent. When activated, HERVs produce viral-like proteins and RNA, which the immune system may mistake as foreign invaders. This molecular mimicry—where the body's own tissues are attacked—lies at the heart of many autoimmune conditions. The implications are profound, suggesting that our genome's viral past could be a hidden driver of modern diseases.
One of the most compelling examples of this phenomenon is seen in multiple sclerosis (MS). Researchers have detected elevated levels of HERV-W envelope proteins in the brains and blood of MS patients. These proteins, known for their inflammatory properties, may disrupt the blood-brain barrier and provoke attacks on myelin, the protective sheath around nerve fibers. While the exact mechanisms remain under investigation, the correlation between HERV activation and MS progression has opened new avenues for therapeutic interventions.
But HERVs are not merely villains in this story. Some studies suggest that these ancient viral sequences have been co-opted by the human body for beneficial functions, such as regulating placental development and modulating immune responses. This duality—both friend and foe—complicates the narrative, highlighting the delicate balance between evolutionary adaptation and disease susceptibility. Understanding this balance is crucial for developing targeted treatments that silence harmful HERV activity without disrupting their potential protective roles.
The hunt for therapies that modulate HERV expression is already underway. Experimental drugs targeting HERV-W proteins, for instance, have shown promise in early clinical trials for MS. Meanwhile, advances in CRISPR gene-editing technology offer the tantalizing possibility of permanently silencing problematic HERV sequences. Yet, ethical and practical challenges loom large. Editing the human genome to remove or suppress viral elements carries unknown risks, and the long-term consequences of such interventions remain speculative.
Beyond autoimmune diseases, the study of HERVs has broader implications for understanding human health. Their activation has been linked to cancers, neurodegenerative disorders, and even psychiatric conditions like schizophrenia. Some researchers speculate that HERVs may act as "evolutionary sensors," responding to environmental pressures by altering gene expression in ways that could either protect or harm the host. Unraveling these connections could revolutionize our approach to medicine, shifting the focus from treating symptoms to addressing the root causes of disease.
As the field progresses, one thing is clear: the line between "self" and "non-self" in our genome is far blurrier than once thought. The viral remnants embedded in our DNA are not passive bystanders but dynamic elements that can influence our biology in unexpected ways. Whether they emerge as allies or adversaries may depend on the intricate interplay between genetics, environment, and chance. For scientists and clinicians, the challenge lies in deciphering this complexity to harness HERVs for good while mitigating their potential for harm.
The story of human endogenous retroviruses is still being written, with each discovery adding new layers to our understanding of autoimmune diseases and beyond. What began as a curiosity—a glimpse into our viral ancestry—has evolved into a cutting-edge frontier of biomedical research. As we continue to explore this hidden dimension of our genome, we may find that the keys to some of medicine's most stubborn puzzles have been lurking within us all along.

By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025